To Our Emergency Medicine Clients and Colleagues
Founder, Edelberg + Associates – February 2023
As we closed the first month of the new 2023 E/M Coding Guidelines for emergency medicine, a number of identified issues arose which will require provider attendance to documentation details on a much larger scale. We noted at some facilities a drop in the percentage of 99285’s that could not be fully offset by the increase in 99283’s. So, now is a great time to recap what is required for 99285!
Nature of Presenting Problem:
1 or more chronic illnesses with severe exacerbation, progression, or sides effects of treatment
Amount and/or Complexity of Data to be Reviewed and Analyzed – Extensive
(Must meet the requirements of a least 2 of 3 categories)
Category 1: Tests, documents or independent historian(s)
Any combination of 3 from the following:
- Review of prior external note(s)from each unique source;
- Review of the result(s) of each unique test;
- Ordering of each unique test;
- Assessment requiring an independent historian(s)
Or
Category 2: Independent interpretation of tests
- Performed by another physician/other qualified health care professional (not separately reported);
Or
Category 3: Discussion of management or test interpretation
Discussion of management or test interpretation with external physician/other qualified health care professional/appropriate source (not separately reported)
High risk of morbidity from additional diagnostic testing or treatment
Examples only:
- Drug therapy requiring intensive monitoring for toxicity
- Decision regarding elective major surgery with identified patient or procedure risk factors
- Decision regarding emergency major surgery
- Decision regarding hospitalization or escalation of hospital-level care
- Decision not to resuscitate or to de-escalate care because of poor prognosis
- Parenteral controlled substances
Documentation Tips:
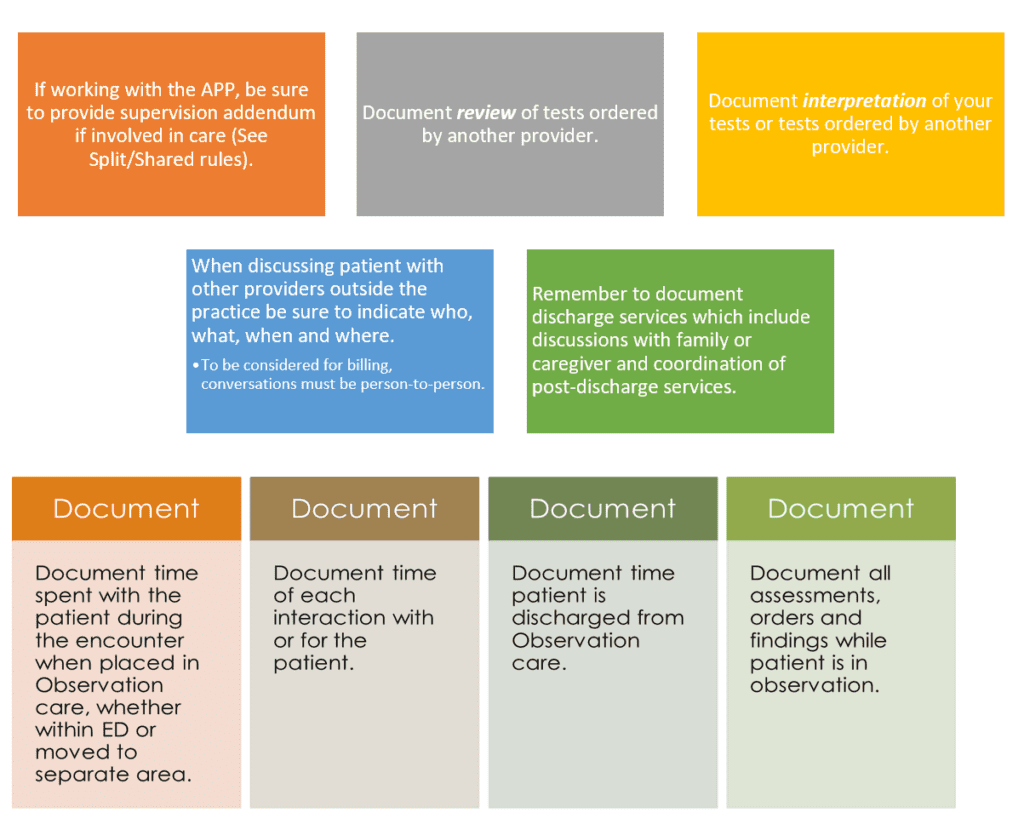
Some Documentation Take-Aways
- Do document differential diagnoses from which the final diagnosis is selected;
- Do document any social determinants of heath that may affect your treatment, disposition, patients ongoing health, etc.
- Do document the details of your discussions (interactive exchange) with other emergency physicians. Discussions with external physicians (from other specialties/other practices) should also be detailed in your documentation.
- Do reference any analysis (included in the thought processes for diagnosis, evaluation, or treatment) of a test vs. interpretation unless interpretation is coded separately. Any test or interpretation coded separately is NOT included in the E/M code level.
- Do provide content of any discussion with family, friends, caregivers, etc. (eg, parent, guardian, surrogate, spouse, witness who provides a history in addition to a history provided by the patient who is unable to provide a complete or reliable history (eg, due to developmental stage, dementia, or psychosis)
- Do develop rule-out/rule-in discussion from HPI/CC/Test results.
- Do use adjectives to describe patient condition, reasons for additional care, etc. (severe, significant, high risk, limited mobility, serious, altered, etc.
- Do remember to document time managing patient care for critical care.
- Do address any additional problems you identify and discuss how they are being managed e.g. diagnostic studies, differential dx, discussion with other providers, etc.
- Do not reference review of tests not ordered or performed, e.g. “ I have reviewed all tests and have discussed with patient and/or family.” Avoid generalized or templated statements if they are not pertinent or accurate.
Posted by: Caral Edelberg on 2/8/23
© 2025 - Edelberg & Associates

